The Basics
What is HPV?
HPV stands for human papillomavirus. It is a common virus and there are over 40 different types of HPV (called "strains") that can be spread through sexual contact.
Some types of genital HPV may cause genital warts, while other types of genital HPV are linked to abnormal cell changes on the cervix (opening to the uterus) and certain cancers.
How common is HPV?
HPV is the most common STD in the United States. It is estimated that at least 79 million people in the US have it. Most sexually active people become infected with HPV at some time in their lives (about half of all men and 3 out of 4 women), usually within the first few years of having sex. Most people clear these infections within a year on their own (within 8 to 13 months), but some infections persist and can progress to cause cancer over a long period (usually around ten years). Clearing an infection means that your body naturally gets rid of the virus and it can't be found in your body by tests anymore.
Where does HPV live?
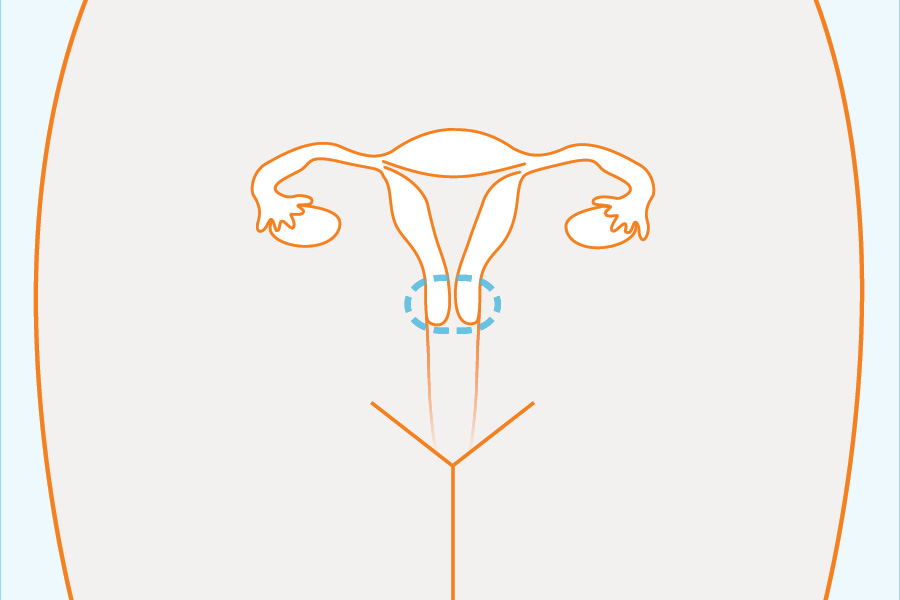
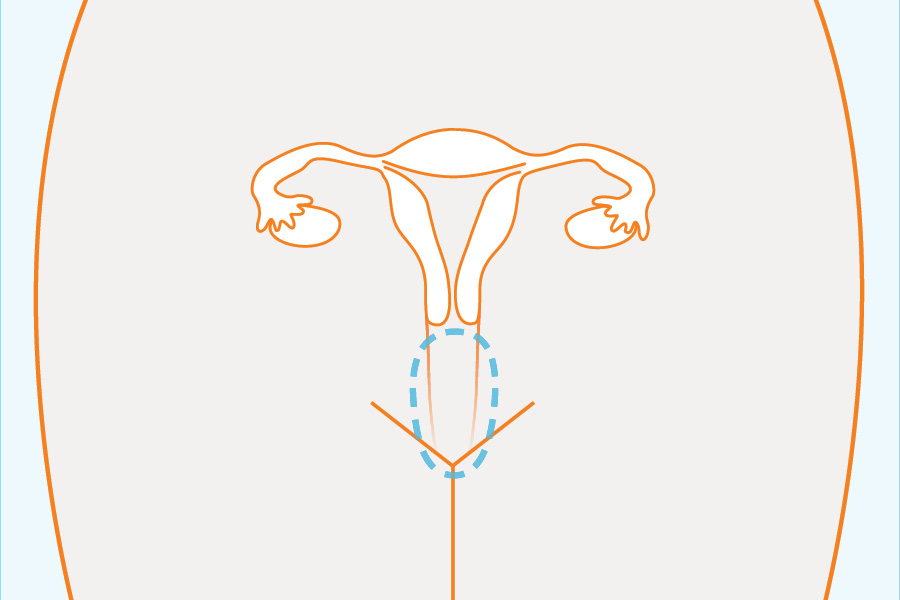
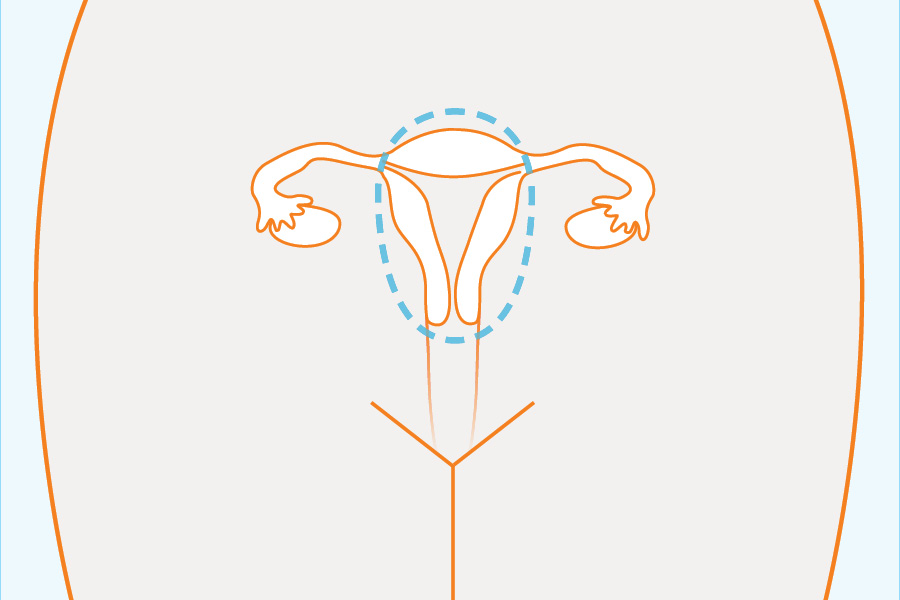
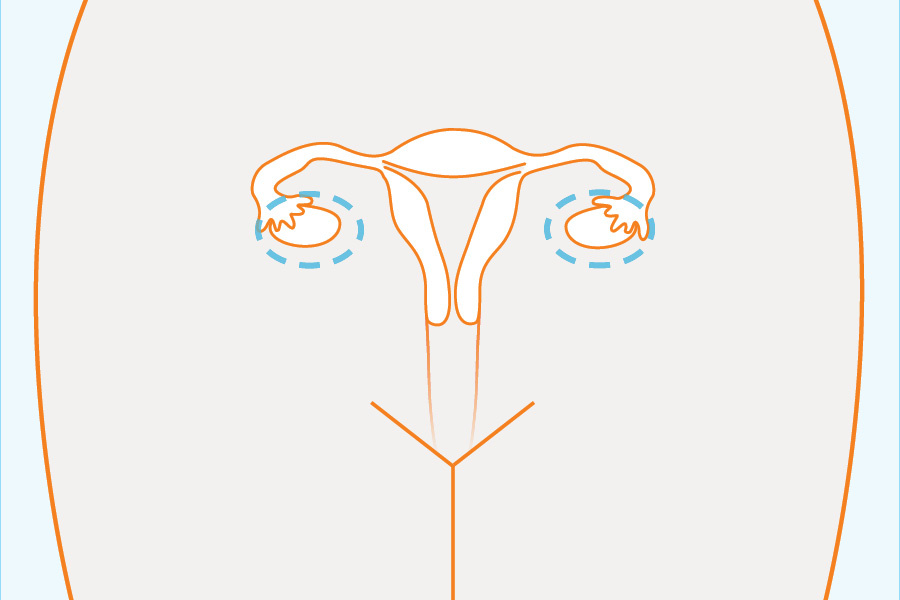
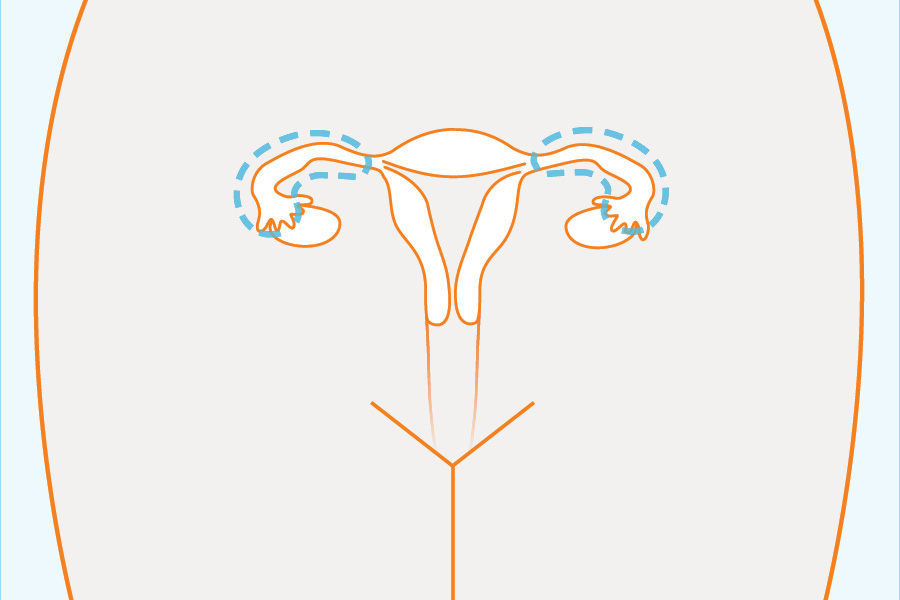
In females:
In males:
- Skin of penis
In males and females:
- Anus
- Rectum (tube leading down to the anus from the intestines)
- Mouth
- Tonsils (in your throat)
Symptoms and Disease
If I have HPV, will I develop symptoms?
Most people with HPV have no symptoms, although the proportion of infected people who develop symptoms is different for different types of HPV.
Often, HPV has symptoms that you won't be able to see. Some types of the virus will cause cells in the cervix (the part of a woman's body between her vagina and her womb/uterus) to change, but you won't notice these symptoms unless your doctor is looking for them.
Other types (called "strains") of HPV will have visible symptoms, like genital warts, but a lot of people who carry the strain for genital-wart-causing HPV still won't have symptoms or will have small warts that they don't notice.
What are the symptoms of HPV?
There are over 100 types of HPV. Different types have different symptoms. Possible symptoms include genital warts, cervical cell changes, and cancers.
Genital warts: Occur in males and females. Warts do NOT lead to cancer. What they look like:
- Warts can be big or small
- Warts may be flesh-colored or white
- Either a single wart, many warts spread out from each other, or clusters of warts
- Warts are flat and only slightly raised from skin
- Warts are smooth or lumpy like a cauliflower
- Warts do not cause itching or burning
For females, warts can be on the:
- Outside of the vagina
- Anus
- Inside of the vagina (rare)
- Cervix (the area between the vagina and the womb/uterus) (rare)
For males, warts can be on the:
- Penis
- Scrotum (skin around testicles)
- Thighs
- Anus
Cervical cell changes (pre-cancerous): Only occur in females. You will not be able to see these symptoms on your own. They can only be detected during a pap smear.
Cervical cell changes are often categorized as low grade and high grade. Low grade cervical cell changes are likely to clear on their own, which means that the body can heal without treatment, and they don't develop into cancer. Higher-grade cell changes are more likely to develop into cancer, and so more tests or procedures might be done.
Cervical cell changes can cause lesions (which look like cuts or sores) on the cervix over time. If untreated, these lesions may become cervical cancer. It is important for females to get screened for cervical cell changes and lesions with a Pap smear every few years.
Cervical cancer: Occurs only in females. Cervical cancer does not usually have the symptoms listed below until someone has had it for a while. Cervical cell changes and lesions (which aren't yet cancer) can sometimes cause cervical cancer if they are not treated.
Symptoms of cervical cancer:
- unusual or heavy bleeding from the vagina
- bleeding between periods
- pain in the lower back
- pain during intercourse
Other HPV-related cancers: These include cancers of the vagina, penis, anus, and oropharynx (back of the throat). You may not have symptoms of these cancers until they are advanced, but a doctor or other healthcare professional can give you more information about them.
How quickly do the symptoms of HPV develop?
Genital warts: Symptoms often appear weeks or months after you get infected, usually between 6 weeks to 6 months. This type of HPV sometimes becomes undetectable (meaning that you will not have warts again and may clear the virus from your body) 1-2 years after symptoms.
Cervical cell changes: Symptoms may appear a long time after you are infected but can be detected with a Pap smear. It is important for females to get screened for cervical cell changes by a gynecologist with a Pap smear every few years.
Cervical cancer: Symptoms of cancer will not appear for a long time after infection with HPV. Most people develop cervical cell changes (see above) before they develop cervical cancer.
Other HPV-related cancers: Symptoms will not appear for a long time after infection with HPV.
What can happen if I don't get treated for HPV?
Genital warts: The warts may not go away for a while (warts only disappear on their own in 10-20% of people). Even if they do go away, you may still be able to transmit genital to warts to people you have sexual contact with.
Cervical cell changes (abnormalities): Many cervical abnormalities will resolve (get better) on their own, but some progress (change) into cervical cancer.
Cervical cancer: Untreated cervical cancer can cause serious illness and death.
Other HPV-related cancers: Untreated cancer can cause serious illness and death.
Transmission
How is HPV spread?
HPV is spread through direct genital-to-genital or oral-genital skin contact. It can be passed without any sharing of fluids. It can be spread through:
- vaginal sex (both partners)
- anal sex (both partners)
- performing oral sex on a man or woman
- genital-genital rubbing (outercourse) between women or between women and men
Genital warts do not appear anywhere other than the genitals, but they are very easy to spread. Most partners of people with genital warts develop them. Newly developed warts are more infectious than older ones.
HPV can be spread even when no symptoms are present. Mother to child transmission is rare.
How can I prevent getting HPV?
Vaccines: Vaccines can protect both females and males from the types of HPV that cause genital warts and cancers. However these vaccines only protect you before you have been exposed to HPV, they do not help you get rid of infections that you already have.
- Females: There are two vaccines that can protect you against some types of HPV. Cervarix protects females from the types of HPV that cause most cervical cancer. Gardasil protects from the types of HPV that cause most cervical cancers and most genital warts. It is recommended that girls get either vaccine at age 11 or 12, and older females up to age 26 who were not vaccinated previously.
- Males: Gardasil protects males against most genital warts and anal cancer. It is recommended that boys get either vaccine at age 11 or 12, and older males up to age 26 who were not vaccinated previously.
Condoms: If you can't get vaccinated, you can lower your risk of getting it by using condoms. Studies have demonstrated that latex condoms help reduce HPV transmission. But remember, since HPV is transmitted through skin-to-skin contact, you can still get it if you come into contact with infected areas that are not covered by condoms.
For more tips, visit our Protect Page.
If I have HPV, how can I prevent giving it to someone else?
Use condoms: You can lower your risk of spreading it by using condoms. Studies have demonstrated that latex condoms help reduce HPV transmission. But remember, since HPV is transmitted through skin-to-skin contact, you can still give it to someone through infected areas that are not covered by condoms.
Get treated: Getting treated for genital warts can lower your chance of infecting others, but will not eliminate it. Treatments include genital wart removal (freezing off the warts) or a liquid medication.
For more tips, visit our Protect Page.
Can I still infect other people with HPV if I don't have symptoms?
Yes, sometimes your genitals (or skin around or in your genitals) can be infected with HPV even if you don't have warts or other symptoms. The same thing is true with anal HPV. Anyone who comes in contact with infected skin can get HPV. It is not clear if you can infect others if you have HPV in your throat.
For how long am I infectious with HPV?
One study (Winer 2011) found that 65% of young women infected with HPV will stop testing positive for that type of HPV one year after the first tested positive for it, and 90% after two years. It's hard to know for sure if that means they stopped being infectious, or whether the same would be true of men or older women.
Am I more infectious with HPV at certain times?
Genital warts: you may be more infectious when you have warts on your skin (especially right after they show up), but there are few studies on this.
HPV DNA, cervical cell changes, or cervical cancer: you are probably more infectious when showing symptoms than when not showing symptoms.
Other types of HPV-related cancers: very little is known.
Tests, Results, & Treatment
How long do I have to wait to get tested for HPV?
If you have symptoms of warts, you should get tested right away. If you are a woman, you should get tested (with a pap smear) starting at age 21 and then once every three years, unless a doctor tells you otherwise.
How do you test for HPV?
Genital warts: To test for genital warts, a doctor or other healthcare professional will ask about your symptoms and look for warts.
HPV DNA: Only women can get tested for HPV DNA, and only on their cervix. Men cannot get this test, and this test cannot detect HPV in places of the body other than the cervix. This test only looks for the types ("strains") of HPV that cause cervical cancer, not the types that cause genital warts. For women being tested, a sample will be usually be taken as part of a Pap smear- part of the sample will be tested for HPV DNA, and part will be tested for cervical cell changes (see below).
Cervical cell changes (pre-cancer): Only women can get tested for cervical cell changes. To test for cervical cell changes, a doctor or other healthcare professional will give you a Pap smear. A Pap smear screens for changes to the cells of the cervix that might cause cancer. If the test detects cell changes, your doctor will refer you for more tests to diagnose what type of changes there are and whether treatment is needed. Pap smears often find cervical cell changes early enough that treatment can be given before cervical cancer develops.
Cervical cancer: Only women can get tested for cervical cancer. To test for cervical cancer, a doctor or other healthcare professional will give you a physical exam, will look at your cervix, and may take a sample of cells (called a biopsy). If you have any symptoms of cervical cancer, make sure you tell your doctor about them.
Other HPV-related cancers: To test for most cancers, a doctor or other healthcare professional will give you a physical exam if you have symptoms. There is no test for penile cancer or oral/pharyngeal (throat) cancer if you don't have symptoms. Some recommend that males who have receptive anal sex (other men's penises in their anus) should have an anal Pap smear, especially if they are HIV positive. Like with cervical cell changes, Pap smears often find anal cell changes early enough that treatment can be given before anal cancer develops. It is not known whether screening for anal cancer improves health outcomes, because often abnormal (not normal) cells in the anus will resolve themselves (the body will heal them) without treatment.
Where can I get tested for HPV?
Genital warts: Visual exams for genital warts can be done by healthcare professionals in STD clinics or by your usual doctor. You'll probably be sent to a dermatologist for treatment. If you actually see the warts on your genitals, you can probably go straight to a dermatologist rather than going to another type of doctor first. Check to make sure your insurance will let you do this first.
HPV DNA: If you're a woman, a gynecologist may be able to test for cervical HPV DNA as a part of your Pap smear.
Cervical cell changes (pre-cancer): Tests for abnormal (not normal) cell changes caused by HPV are usually done by gynecologists as part of a Pap smear. Other tests to determine exactly what type of cell changes you're having are also usually done by gynecologists.
Cervical cancer: Cervical cancer is usually diagnosed by a cancer specialist (called an oncologist).
Other: Other tests for abnormal (not normal) cell changes caused by HPV, or HPV-related cancers are usually done by a urologist (if you're a man), general care provider, or cancer specialist (called an oncologist).
To find doctors of all these different types who take your health insurance, visit our Test Page.
What do my HPV test results mean?
You are diagnosed with genital warts: This means you have the form of HPV that causes genital warts. Your doctor will let you know how and when you should treat the genital warts. This is does NOT mean you have the same type (strain) of HPV that causes cancer.
You test positive for HPV DNA: This means that you have one of the strains of HPV that can cause cervical cancer. This does not mean that you will necessarily develop cervical cancer. It does mean that you're probably infectious (if a man has vaginal sex with you, he might get HPV too).
You test positive for cervical cell abnormalities: Your doctor may tell you that you have an abnormal Pap smear. This just means that your cervical cells look different than normal cervical cells. It does not mean you necessarily have cancer. Your doctor will tell you what to do next. They may want to look closer at the cells on your cervix by doing a colposcopy and biopsy (a quick procedure that lets them look more carefully at the cells on your cervix) or they may suggest you come in for another Pap smear soon. You can read more about interpreting your test results here.
Is HPV curable?
No, HPV is not curable. However, in many cases your body can clear HPV (meaning that your body can get rid of it itself). Just because you don't have warts or other symptoms doesn't mean the infection is gone from your body.
What should I expect in terms of treatment?
Discuss treatment options with a doctor or other healthcare professional.
Genital warts: Warts can be treated, which may reduce the risk of transmission to another partner and can get rid of symptoms. There are many methods of treating genital warts, including:
- cryotherapy (freezing off the warts with liquid nitrogen)
- chemical therapies applied to the surface of the wart
- cutting off warts
- burning off warts with an electrical current
- using an intense laser to destroy warts
- creams designed to boost the immune system to fight HPV
- gels that destroys the tissue of external genital warts
Even if the warts are gone, you can still transmit the virus.
Cervical cell changes: Usually cervical cell changes can heal on their own, so your doctor may just want to monitor them. If the cell changes cause lesions on your cervix, your doctor might decide to treat you with:
- cryotherapy (freezing the cells with liquid nitrogen)
- LEEP (Loop Electrosurgical Excision Procedure)
- conization (also called a cone biopsy, where a cone shaped piece of tissue is removed from the cervix)
- using an intense laser to destroy cells
Cervical cancer: Cervical cancer has a variety of treatment options.
Other HPV-related cancers: Cancer has a variety of treatment options.
Can I use medication I already have to treat HPV?
No. Do not use over-the-counter wart treatments in the genital area.
Can I share my HPV medication with my partner?
No. They should see a doctor or other healthcare professional to get their own treatment.
Partner Notification
Should I notify my partner(s) if I have HPV?
Maybe, if you feel safe doing so. HPV is a very common infection, and it is very hard to know who gave it to you or who you gave it to. It's really hard to test for, especially in men, so notifying your partner may cause them to worry about something that they can't get tested for.
Who should I notify if I have HPV?
Below is our take on which of your partners to notify. There aren't great formal guidelines on any of this.
Past Partners: As far as we know, there are no clear recommendations for notifying your past partners. If you've had more than one partner, it's hard to know which partner infected you. it is also hard to figure out who you infected. Also, because so many infections clear on their own, chances are that by the time you are diagnosed with HPV, whoever gave it to you will not be infectious anymore. Your past partners, even if they are infected, probably do not have symptoms and have no easy way of getting tested (when there aren't any symptoms). It is difficult to give clear recommendations because there is a lot we don't know about HPV. In general, physicians don't recommend notifying past partners, but it's up to you.
Current Partners: If you have just been diagnosed with HPV, you may want to tell your current partners. You are probably shedding the virus (which means, live virus is on the surface of your skin and other infected areas), and you are most likely to spread HPV when you are shedding the virus. If you tell your partner, they can get vaccinated and you can use condoms together. If you have genital warts, and tell your partners, they might be more likely to watch for warts more carefully, use condoms with other partners, or ask other partners to get vaccinated. If you get diagnosed with cervical HPV DNA, cervical cell changes, or HPV-related cancer and tell your partners, they might be more likely to get screened (if they are someone who can get screened), use condoms, or ask their partners to get vaccinated in the future.
Future Partners: Once people stop showing symptoms, we don't know when or if they stop being infectious. You can still have the virus on your skin or in your reproductive system without warts or visible lesions. If you want to tell your partners, you can bring it up by asking them if they have been vaccinated. If they say "no," you can suggest that they get vaccinated. If you tell your future partners about your infection, they can decide how they want to protect themselves- either with the vaccine, a condom, or abstinence.
That's a lot of people to notify. Which of my partners are most at risk for HPV?
If you have genital warts, we think your most at-risk partners are the ones you had sex with while or just before your warts appeared. This is because we know you had the virus then- we don't really know if you're more infectious when showing symptoms.
If you have cervical HPV DNA, cervical cell changes, or cervical cancer, your current partners are probably most at risk because you're likely to be shedding the virus. The same would probably be true of other HPV-related cancers, but there aren't many studies on those.